Colorectal cancer (CRC) is the second leading cause of cancer-related mortality.[1] Most CRCs develop from the stepwise acquisition of molecular abnormalities along the adenoma-carcinoma and serrated pathways.[2-4] This pathogenic trajectory presents a strategic window for the potential prevention of CRC through endoscopic resection of pre-malignant polyps.
In addition, newer endoscopic techniques can also provide curative resection for some early colorectal and other gastrointestinal cancers, offering a minimally invasive, organ-sparing approach, sparing patients the need for more invasive surgery.[5]
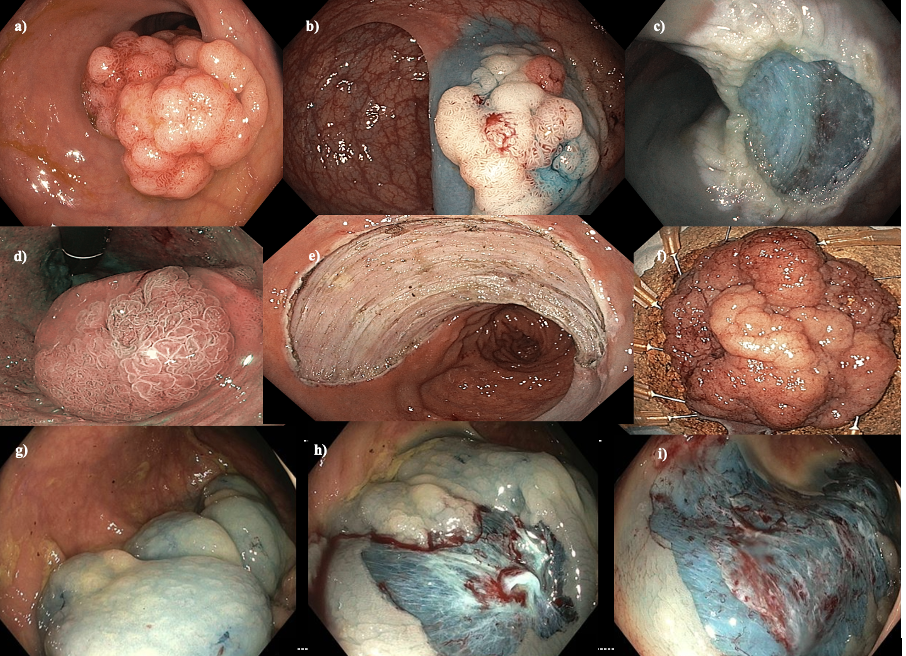
The risk of overt and covert (hidden) cancer in a lesion is dependent on a detail assessment of morphology, size and location in the colon.[7]
Most colonic polyps are <10mm in size and can be safely and effectively removed with a simple, safe and effective cold snare technique. [6] However, Larger lesions >20mm, which comprise approximately 1% of all colorectal lesions may require newer endoscopic techniques for successful removal and may have a greater risk of malignancy.
Endoscopic Mucosal Resection (EMR) and Endoscopic Submucosal Dissection (ESD) are two of the primary methods employed in this domain (Figure 1). EMR is typically used for smaller, well-defined lesions. It involves the injection of a solution into the submucosa beneath the lesion to create a cushion, facilitating the safe capture and snaring of the lesion for resection. Large lesions need to be removed in more than one piece (piecemeal) and as such, this technique is suited to lesions with a low risk of covert cancer due to a small but not insignificant risk of leaving viable tissue behind.
For higher risk lesions, ESD offers a more advanced approach, allowing for the en-bloc resection. This technique is more time-consuming and technically demanding than ESD. Akin to microsurgery, it involves dissecting the submucosal layer beneath the lesion with the aim of achieving a complete resection in one single piece with curative intent
The combination of high-quality research with device innovations have allowed for great advancements to endoscopic resection techniques resulting in improved patient outcomes with lower morbidity and mortality rates.
The above techniques are performed both by Dr Joshua Butt and Dr Oliver Cronin. Both are happy to be contacted about suitability of specific cases.
1. Patel SG, Karlitz JJ, Yen T, et al. The rising tide of early-onset colorectal cancer: a comprehensive review of epidemiology, clinical features, biology, risk factors, prevention, and early detection. Lancet Gastroenterol Hepatol. 2022;7(3):262-74.
2. Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134(5):1570-95.
3. Kedrin D, Gala MK. Genetics of the serrated pathway to colorectal cancer. Clin Transl Gastroenterol. 2015;6(4):e84.
4. Itzkowitz SH, Yio X. Inflammation and cancer IV. Colorectal cancer in inflammatory bowel disease: the role of inflammation. Am J Physiol Gastrointest Liver Physiol. 2004;287(1):G7-17.
5. Cronin O, Bourke MJ. Endoscopic Management of Large Non-Pedunculated Colorectal Polyps. Cancers (Basel). 2023;15(15).
6. Kaltenbach T, Anderson JC, Burke CA, et al. Endoscopic Removal of Colorectal Lesions: Recommendations by the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2020;115(3):435-64.
7. Cronin O, Sidhu M, Shahidi N, et al. Comparison of the morphology and histopathology of large nonpedunculated colorectal polyps in the rectum and colon: implications for endoscopic treatment. Gastrointest Endosc. 2022;96(1):118-24.
8. Burgess NG, Hourigan LF, Zanati SA, et al. Risk Stratification for Covert Invasive Cancer Among Patients Referred for Colonic Endoscopic Mucosal Resection: A Large Multicenter Cohort. Gastroenterology. 2017;153(3):732-42.e1.