In October 2023, updates were made to the NHMRC-endorsed clinical guidelines regarding bowel cancer screening. These revisions aim to enhance the effectiveness of screening strategies and improve outcomes for those at increased risk.
The updated guidelines emphasise the importance of tailoring screening recommendations based on an individual’s specific risk factors, including their family history of bowel cancer. Research indicates that individuals with one or more first-degree relatives (FDRs, defined as a parent, sibling, or child) who have been diagnosed with bowel cancer are at higher risk themselves. Therefore, proactive screening measures are crucial in detecting the disease at an early and treatable stage.
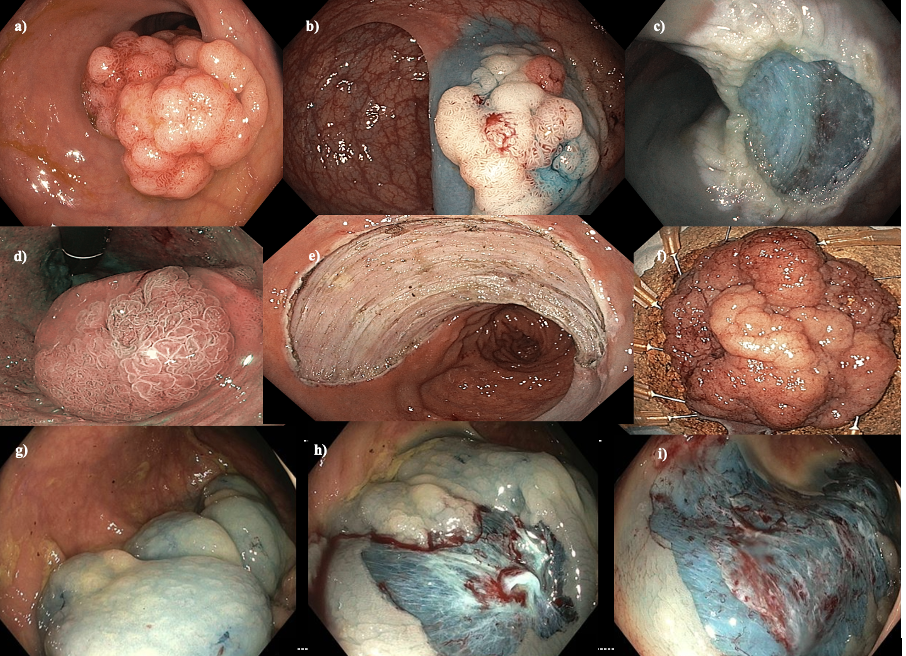
Patients with 2 or more FDRs with bowel cancer should have at least 5 yearly screening colonoscopies starting at an age of 10 years younger than their youngest FDR or age 50, whichever is younger. Patients with 3 FDRs with bowel cancer should start at least 5-yearly screening colonoscopies at an age 10 years younger than their youngest FDR or age 40, whichever is younger. This proactive approach allows for the timely detection of precancerous polyps or early-stage cancer, which can significantly improve treatment outcomes and overall prognosis.
In addition to colonoscopy, alternative screening modalities such as fecal occult blood testing (FOBT) or fecal immunochemical testing (FIT) may be recommended based on individual circumstances and preferences. These non-invasive tests can serve as valuable adjuncts to colonoscopy or as interim screening measures between colonoscopy intervals.
The new recommended age for FOBT screening is now 45 for patients at an average risk of risk of bowel cancer.
These updated clinical guidelines emphasise the importance of personalised risk assessment for individuals with a family history of bowel cancer. The new recommendations aim to enhance early detection rates, and ultimately reduce the burden of bowel cancer in Australia.