Introduction
Constipation is a common complaint that we encounter regularly. The term “constipation” can mean different things to different people. Here, we provide an approach to diagnosing and treating constipation.
Take a history to determine what is meant by constipation
The word ‘constipation’ is used often for many different symptoms. Sometimes in reference to hard stools, sometimes straining (but the stools aren’t necessarily hard). Some patients can present with right-sided abdominal pain due to faecal loading, or severe bloating, without always having typical constipation symptoms of hard stool or straining. The approach then changes a bit depending on what symptom they have.
For consideration :
- Some patients have bloating due to faecal loading rather than food intolerances. If someone doesn’t respond to a low FODMAP diet for bloating, think about constipation (along with many other causes of bloating!). If there is any suspicion of constipation, the preference is to treat the constipation prior to commencing a low FODMAP diet.
- Some patients with constipation also have diarrhoea. This can be due to intermittent laxative use that causes diarrhoea; or in the setting of constipation, where faecal loading causes over-activation of the bowel contractions, resulting in diarrhoea. Typically, the story is one of, 1-2 days of having no bowel action or hard bowel actions, then 1-2 days of diarrhoea, followed by 1-2 days of constipation etc.
If they have constipation …
Clarify what they mean, then check for underlying medical or surgical causes such as:
- Medications
- High calcium levels
- Hypothyroidism
- Inflammatory Bowel Disease (IBD)
- Immobility
In regards to treating constipation, aside from the underlying disease, we can think about –
1. Stool Consistency
People tend to have enough soluble fibre in their diet (assuming they eat fruit and vegetables), but it is often hard to have enough insoluble fibre. So, if the stool is hard, we recommend starting with Chia seeds or Phloe capsules. Usually low dose, then slowly increase. Phloe capsules and chia seeds are both mostly insoluble fibre, so don’t cause or contribute to bloating. They are also safe to use long term, safe in pregnancy and in people with coeliac disease.
- Chia Seeds: Start with a low dose of 1/4 to 1/2 teaspoon and gradually increase. We have a delicious chia seed pudding recipe that we share with our patients.
- Phloe Capsules: Made from kiwi fruit, start with one capsule.
If these don’t work to soften the stool, adding in a soluble fibre may help (most of the fibres at the supermarket/pharmacy are soluble fibres – Metamucil/psyllium, Benefibre, prunes).
The next step is usually osmotic laxatives such as Movicol or Osmolax. These are more prone to causing diarrhoea than fibres. Stimulant laxatives such as Senna-containing products, or Bisacodyl, would often be used later as they can cause abdominal pain due to the increase in colonic contractions.
Please note :
- Slim tea/laxative teas often contain Senna. Often it is better to avoid these if possible as the dose can be so variable depending on the water temperature, the length of time the tea is brewed etc.
- Education for patients in use of fibre/laxatives is important, rather than reacting to constipation then treating it intermittently, they are better off taking a small amount of fibre/laxatives regularly to prevent constipation.
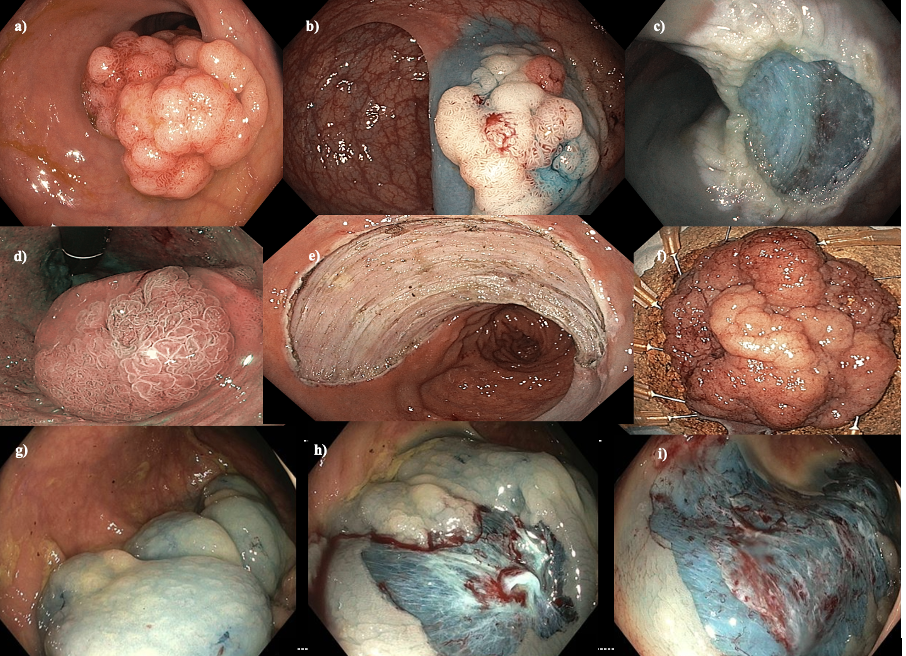
- Despite previous teaching, laxatives long term are safe. The concern about dependance was based upon a single case report in the 1980’s of a patient who was taking extraordinarily large doses of stimulant laxatives. Fibre and other laxatives don’t change the bowel function, although stimulant laxatives can causing staining of the bowel which clinically is meaningless, except for altered appearance on colonoscopy.
2. Pelvic floor/defecation function
Pelvic floor function is a vital part of defecation. There can be many issues that occur including weakness, discoordination and altered sensation of the rectum. With weakness of the pelvic floor, or hard stools, often the abdominal muscles can be used during defecation, leading to activation of the anal sphincter muscles (rather than relaxation). People can feel like they are straining against a closed anus, or may pass thin stools. Other symptoms can include straining with a feeling of weakness, faecal urgency but low volume (due to altered rectal sensation), and a feeling of incomplete emptying.
Pelvic floor physiotherapy can assess and improve this considerably, specifically one with an interest in bowel health.
For consideration :
- There are other causes of thin stools, straining, urgency and low volume stools, such as rectal cancer and inflammatory bowel disease (IBD).
3. Assessment of GI Tract Speed
An assessment may diagnose slow transit constipation. Treatment options include treating the underlying cause, bowel motility medication, regular enemas, electrical stimulation therapy or surgery.
Often the first two approaches will do the trick and there will be no need to assess GI tract speed.
Conclusion
Managing constipation requires a multi-faceted approach that begins with understanding the patient’s symptoms and ruling out underlying causes. By focusing on stool consistency, pelvic floor function initially, we can offer effective treatment for this common condition.